Rosuvastatin is a generic prescription drug that’s used to treat high cholesterol and reduce the risk of heart disease. Rosuvastatin comes as an oral tablet and belongs to a group of drugs called statins.
Rosuvastatin is available as the brand-name drug Crestor. It’s also available as a generic drug. Generic drugs usually cost less than the brand-name version. In some cases, they may not be available in every strength or form as the brand-name drug.
This drug may be used as part of a combination therapy. This means you may need to take it with other medications.
Why it’s used
Rosuvastatin is used to reduce your LDL (bad) cholesterol levels and increase your HDL (good) cholesterol levels. It also reduces your triglyceride levels. (Triglycerides and cholesterol are types of lipids, or fats, in your blood.)
Reducing your cholesterol levels helps prevent blockages from forming in your arteries. These blockages can cause serious problems, including heart attack or stroke.
Specifically, doctors prescribe rosuvastatin to:
- Reduce LDL in adults with the following conditions, when prescribed with a low cholesterol diet:
- high cholesterol
- high triglycerides
- type 3 hyperlipoproteinemia, also referred to as dysbetalipoproteinemia (a genetic disorder that prevents the breakdown of lipids in the body)
- narrowing of arteries due to cholesterol buildup, to help slow the worsening of this condition
- Reduce LDL in adults and some children with heterozygous familial hypercholesterolemia, a genetic condition that causes high cholesterol. For this use, rosuvastatin is prescribed with a low cholesterol diet.
- Reduce LDL in adults and some children with homozygous familial hypercholesterolemia, a genetic condition that causes high cholesterol. For this use, rosuvastatin may be taken alone or together with other medications that lower LDL.
- Help prevent heart disease in certain adults. Heart disease can lead to major cardiovascular events, such as heart attack or stroke.
How it works
Rosuvastatin belongs to a class of drugs called statins. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Rosuvastatin works by blocking enzymes in your liver that make cholesterol. This lowers your levels of LDL (bad) cholesterol. It also raises your levels of HDL (good) cholesterol.
Rosuvastatin can cause mild or serious side effects. The following list contains some of the key side effects that may occur while taking rosuvastatin. This list does not include all possible side effects.
For more information on the possible side effects of rosuvastatin, or tips on how to manage a bothersome side effect, talk with your doctor or pharmacist.
More common side effects
The more common side effects that can occur with use of rosuvastatin include:
- headache
- pain in the abdomen
- muscle pain
- nausea
- weakness
If these effects are mild, they may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency. Serious side effects and their symptoms can include the following:
- Severe muscle problems. Symptoms can include:
- unexplained or unusual muscle pain
- weakness
- fever
- Liver problems. Symptoms can include:
- unexplained or unusual weakness
- decrease in appetite
- pain in the abdomen
- dark urine
- yellowing of the skin or the whites of the eyes
Rosuvastatin can interact with several other medications. Different interactions can cause different effects. For instance, some can interfere with how well a drug works, while others can cause increased side effects.
The following text gives examples of medications that can interact with rosuvastatin. These are not all of the drugs that may interact with rosuvastatin.
Before taking rosuvastatin, be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Acid-reducing drugs
When taken with rosuvastatin, certain antacids that contain aluminum or magnesium can decrease the amount of rosuvastatin in your blood. This makes it less effective, and it won’t work as well to treat your condition. These drugs should be taken at least 2 hours after taking rosuvastatin. Examples of these drugs include:
- aluminum hydroxide
- magnesium hydroxide
Blood thinner
Warfarin (Jantoven) is used to thin the blood. Taking this drug with rosuvastatin can affect how quickly your blood clots. Your doctor may monitor your body’s ability to form blood clots more often when you start taking rosuvastatin or if your doctor changes your dosage. They’ll do this by ordering certain blood tests.
Cholesterol drugs
When taken with rosuvastatin, some other drugs used to treat high cholesterol can increase the levels of rosuvastatin in your blood. This raises your risk of muscle problems. Before taking these drugs, make sure your doctor knows that you take rosuvastatin. Examples of these drugs include:
- niacin (Niacor)
- gemfibrozil (Lopid)
- fenofibrate (Tricor)
HIV drugs
When taken with rosuvastatin, certain drugs used to treat HIV can increase levels of rosuvastatin in your body. This raises your risk of side effects from rosuvastatin. These side effects include muscle problems such as muscle pain, weakness, or tenderness.
Examples of these drugs include protease inhibitors such as:
- atazanavir (Reyataz)
- lopinavir
- nelfinavir (Viracept)
- ritonavir (Norvir)
Hepatitis C drugs
When taken with rosuvastatin, certain drugs used to treat hepatitis C can increase levels of rosuvastatin in your body. This raises your risk of side effects from rosuvastatin, such as muscle problems.
Examples of these drugs include protease inhibitors such as:
- elbasvir/grazoprevir (Zepatier)
Immune suppression drug
Cyclosporine (Gengraf) is used to decrease the strength of the immune system. Using this drug with rosuvastatin can increase levels of rosuvastatin in your body. This raises your risk of side effects from rosuvastatin, such as muscle problems.
Gout drug
Colchicine (Colcrys) is used to treat gout. Using this drug with rosuvastatin can increase your risk of side effects such as muscle pain and rhabdomyolysis (breakdown of muscle that’s damaged).
Cancer drugs
Darolutamide (Nubeqa) is used to treat prostate cancer. Using this drug with rosuvastatin can increase the levels of rosuvastatin in your body. This raises your risk of side effects from rosuvastatin, such as muscle problems.
Regorafenib (Stivarga) is used to treat cancer of the colon and rectum. Using this drug with rosuvastatin can increase the levels of rosuvastatin in your body, raising your risk of side effects from rosuvastatin.
The rosuvastatin dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re taking rosuvastatin to treat
- your age
- other medical conditions you may have
Typically, your doctor will start you on a low dosage and adjust it over time to reach the dosage that’s right for you. They’ll ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Drug forms and strengths
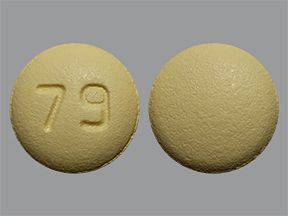
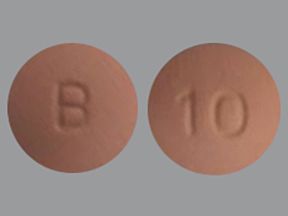
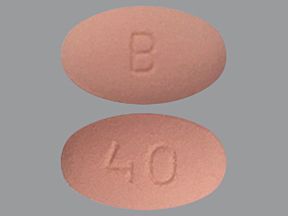
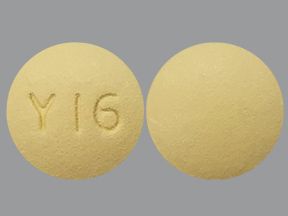
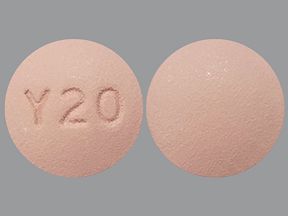
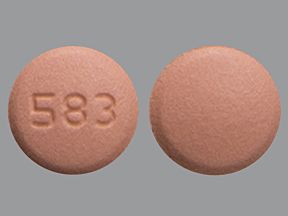
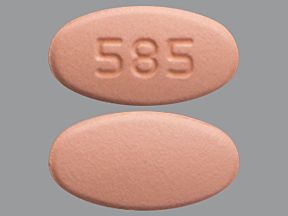
Generic: Rosuvastatin
- Form: oral tablet
- Strengths: 5 milligrams (mg), 10 mg, 20 mg, 40 mg
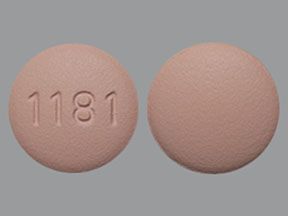
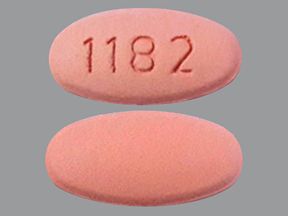
Brand: Crestor
- Form: oral tablet
- Strengths: 5 mg, 10 mg, 20 mg, 40 mg
Dosage for high cholesterol, high triglycerides, dysbetalipoproteinemia, or narrowing of arteries
Adult dosage (ages 18 to 64 years)
- Typical dosage: 5 to 40 mg once daily.
Child dosage (ages 0 to 17 years)
This medication has not been studied in children for this purpose. It should not be used in people younger than age 18 years.
Older adult dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause the body to process drugs more slowly. As a result, a higher amount of a drug stays in the body for a longer time. This increases the risk of side effects.
If you are age 65 years or older, your doctor may start you on a lowered dosage or a different medication schedule. This can help keep levels of this drug from building up too much in your body.
Dosage for heterozygous familial hyperlipidemia
Adult dosage (ages 18 to 64 years)
- Typical dosage: 5 to 40 mg once daily.
Child dosage (ages 10 to 17 years)
- Typical dosage: 5 to 20 mg once daily.
Child dosage (ages 8 to 9 years)
- Typical dosage: 5 to 10 mg once daily.
Child dosage (ages 0 to 7 years)
This medication has not been studied in young children for this purpose. It should not be used in children younger than age 8 years.
Older adult dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause the body to process drugs more slowly. As a result, a higher amount of a drug stays in the body for a longer time. This increases the risk of side effects.
If you are age 65 years or older, your doctor may start you on a lowered dosage or a different medication schedule. This can help keep levels of this drug from building up too much in your body.
Dosage for homozygous familial hyperlipidemia
Adult dosage (ages 18 to 64 years)
- Typical starting dosage: 20 to 40 mg once daily.
Child dosage (ages 7 to 17 years)
- Typical dosage: 20 mg once daily.
Child dosage (ages 0 to 6 years)
This medication has not been studied in young children for this purpose. It should not be used in children younger than age 7 years.
Older adult dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause the body to process drugs more slowly. As a result, a higher amount of a drug stays in the body for a longer time. This increases the risk of side effects.
If you are age 65 years or older, your doctor may start you on a lowered dosage or a different medication schedule. This can help keep levels of this drug from building up too much in your body.
Dosage for heart disease prevention
Adult dosage (ages 18 to 64 years)
- Typical dosage: 5 to 40 mg once daily.
Child dosage (ages 0 to 17 years)
This medication has not been studied in children for this purpose. It should not be used in people younger than age 18 years.
Older adult dosage (ages 65 years and older)
The kidneys of older adults may not work as well as they used to. This can cause your body to process drugs more slowly. As a result, a higher amount of a drug stays in your body for a longer time. This increases your risk of side effects.
Your doctor may start you on a lowered dosage or a different medication schedule. This can help keep levels of this drug from building up too much in your body.
Special dosage considerations
For people of Asian descent: If you are of Asian descent, your body may process this drug differently. This may lead to increased levels of this drug in your blood. Your doctor will likely give you a starting dosage of 5 mg once daily.
For people with kidney disease: Kidney disease can cause the body to process drugs more slowly. As a result, a higher amount of a drug stays in the body for a longer time. This increases the risk of side effects. If you have kidney disease, your doctor will likely give you a starting dosage of 5 mg daily. Your doctor may later increase your dosage to 10 mg daily.
This drug comes with several warnings.
Allergic reaction
This drug can cause a severe allergic reaction. Symptoms can include:
- rash
- hives
- swelling of your face, mouth, and tongue
- difficulty breathing
If you develop these symptoms, call 911 or go to the nearest emergency room.
Don’t take this drug again if you’ve ever had an allergic reaction to it. Taking it again could be fatal (cause death).
Severe muscle problems
This medication can cause severe muscle problems. These include myopathy, with symptoms such as muscle pain, tenderness, or weakness. Myopathy can
If you notice unusual pain or weakness in your muscles, especially if you feel more tired than usual or have a fever, call your doctor right away. Your doctor may decide to stop your treatment with this medication. Call your doctor right away if muscle problems last after your doctor has told you to stop taking this drug.
Liver problems
This drug can increase levels of your liver enzymes. Increased liver enzymes can be a sign of liver damage. Your doctor may check these levels to make sure that this drug is not harming your liver.
Alcohol interaction
Consuming alcohol can increase your risk of liver problems from rosuvastatin. Tell your doctor if you drink more than two glasses of alcohol per day. Be sure to talk with your doctor if you have active liver disease or a history of liver problems.
Warnings for people with certain health conditions
For people with liver problems: Taking rosuvastatin can cause a higher risk of severe muscle problems in people with liver problems. If you have a liver problem, talk with your doctor about whether this drug is safe for you.
For people with kidney problems: There is a higher risk of severe muscle problems in people with kidney problems who take rosuvastatin. If you have a kidney problem, talk with your doctor about whether this drug is safe for you.
Warnings for other groups
For people of Asian descent: If you are of Asian descent, your body may process this drug differently. This may lead to increased levels of this drug in your blood. Your doctor may start you at a lower dosage of rosuvastatin.
For pregnant people: You should not take this drug if you are pregnant or planning to become pregnant. Rosuvastatin can cause fetal harm or end a pregnancy. If you become pregnant, stop taking this medication right away and call your doctor.
For people who are breastfeeding: This drug can pass into breast milk and may cause side effects in a child who is breastfed. You should not breastfeed your child while taking this drug. Talk with your doctor if you breastfeed your child. They can discuss ways to safely feed your child while taking rosuvastatin.
For older adults: The kidneys of older adults may not work as well as they used to. This can cause the body to process drugs more slowly. As a result, a higher amount of a drug stays in the body for a longer time, raising the risk of side effects from this drug. If you are age 65 years or older, your doctor will monitor you closely for side effects while you take this drug.
For children: For several of the conditions rosuvastatin is prescribed to treat, this medication should not be taken by people younger than age 18 years. It can be used in children ages 8 to 17 years to treat heterozygous familial hypercholesterolemia. It can also be used in children ages 7 to 17 years to treat homozygous familial hypercholesterolemia.
Rosuvastatin oral tablet is used for long-term treatment. It comes with risks if you don’t take it as prescribed.
If you stop taking the drug suddenly or don’t take it at all: Your cholesterol may not be managed. Over time, high cholesterol can lead to serious health problems such as a heart attack or stroke.
If you miss doses or don’t take the drug on schedule: Your medication may not work as well as it should or may stop working completely. For this drug to work well, a certain amount needs to be in your body at all times.
If you take too much: You could have dangerous levels of the drug in your body. Symptoms of an overdose of this drug can include:
- severe pain in the abdomen
- vomiting
- diarrhea
- muscle pain and weakness
If you think you have taken too much of this drug, call your doctor or seek guidance from America’s Poison Centers at 800-222-1222 or through its online tool. If symptoms are severe, call 911 or go to the nearest emergency room right away.
What to do if you miss a dose: Take your dose as soon as you remember. But if you remember just a few hours before your next scheduled dose, take your dose at the usual time.
You should not try to catch up by taking two doses at once. This could result in dangerous side effects. Do not take more than one dose of this drug within 12 hours.
How to tell whether the drug is working: Your LDL (bad) cholesterol levels should go down, and your HDL (good) cholesterol levels should go up. You won’t be able to tell that the drug is working. Your doctor will order blood tests to check your cholesterol levels.
Whether you have health insurance or not, cost may be a factor when you’re considering rosuvastatin. What you’ll pay for rosuvastatin may depend on several things, such as your treatment plan and the pharmacy you use.
Here are a few things to consider regarding cost:
- Cost information and savings coupons: You can visit Optum Perks to get price estimates of what you’d pay for rosuvastatin when using coupons from the site. (Note: Optum Perks coupons cannot be used with any insurance copays or benefits.)
- Financial and insurance assistance: If you need financial support to pay for rosuvastatin, or if you need help understanding your insurance coverage, help is available. Consider looking into websites that offer cost resources and information. Two such organizations are NeedyMeds and Medicine Assistance Tool.
Keep these considerations in mind if your doctor prescribes rosuvastatin for you.
General
- You can take this drug with or without food. Taking it with food may help reduce any symptoms of an upset stomach.
- Take this drug at the time(s) recommended by your doctor.
- Do not cut or crush the tablet.
Storage
- Keep this drug at room temperature between 68°F and 77°F (20°C and 25°C).
- Do not store this medication in moist or damp areas, such as bathrooms.
Refills
A prescription for this medication is refillable. You should not need a new prescription for this medication to be refilled. Your doctor will write the number of refills authorized on your prescription.
Travel
When traveling with your medication:
- Always carry your medication with you. When flying, never put it into a checked bag. Keep it in your carry-on bag.
- Don’t worry about airport X-ray machines. They can’t harm your medication.
- You may need to show airport staff the pharmacy label for your medication. Always carry the original prescription-labeled container with you.
- Don’t put this medication in your car’s glove compartment or leave it in the car. Be sure to avoid doing this when the weather is very hot or very cold.
Clinical monitoring
Your doctor will monitor your health during treatment with this drug. You will have blood tests to check your:
- Cholesterol levels: This test will help make sure that this drug is working to improve your cholesterol levels.
- Liver enzymes: Your doctor may check your liver enzymes before and during your treatment with this drug. Your doctor will check them carefully if they think you have liver problems. Let your doctor know if you have symptoms such as unusual muscle pain, tiredness, weakness, or loss of appetite. Also mention if you have pain in the right side of your abdomen, dark urine, or yellowing of your skin or the whites of your eyes.
Your diet
Before you start taking this drug, your doctor may start you on a special diet to lower your cholesterol.
There are other drugs available to treat your condition. Some may be better suited for you than others. Talk with your doctor about other drug options that may work for you.
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.