The more you know about how eating affects blood sugar, the better you can keep your blood sugar managed and lower your risk of diabetes complications.
If you have diabetes, your carbohydrate intake is the most important part of your diet to consider when it comes to managing your blood sugar levels.
The carbs you consume turn into blood sugar. The more carbohydrates you eat, the higher the levels of sugar you’ll have as you digest and absorb your food.
The foods that generate the biggest spike in your blood sugar are those that are high in processed carbohydrates, like refined sugar and flour.But sticking to fiber-packed, whole-food meals and snacks can do wonders to keep your blood sugar steady all day. To learn more, consider signing up for our free Diabetes Nutrition Micro-Lessons.
With diabetes, the body can’t effectively process carbohydrates, aka carbs.
Normally, when you eat carbs, they’re broken down into small units of glucose, which end up as blood sugar.
But not all carbs are created equal. The carbs in fiber won’t spike your blood sugar when you have diabetes, whereas refined carbs, like added sugar and white flour, are more likely to.
Eating low carb can help. Research has shown that people with diabetes can experience long-term improvements in managing blood sugar while eating low carb diets, including keto diets.
Some people use carb counting to help manage their blood sugar levels. To do this, you add up the number of grams of carbs that you eat during each meal and try to keep your carb count under a certain level. You may be able to subtract some fiber grams from total carbs and track what’s called “net carbs.”
The short answer is that you want to choose foods that help keep your blood sugar levels in range.?
The way to gauge this is to check your blood sugar levels after you eat. The way you respond to the foods you eat is unique to you and can vary depending on the situation.
In general, it’s best to avoid foods that are more likely to spike your blood sugar, including refined grains, baked goods like crackers and cakes, juice and sugar-sweetened drinks, and sweets.
Instead, focus on proteins, fats, and low sugar, fiber-rich foods — like low glycemic fruits and vegetables.
You can get medical devices that help monitor and manage your blood sugar levels, including blood glucose monitors (and continuous glucose monitors), insulin pens and pumps, and smart closed loop tech that monitors your blood sugar and delivers insulin automatically as needed.
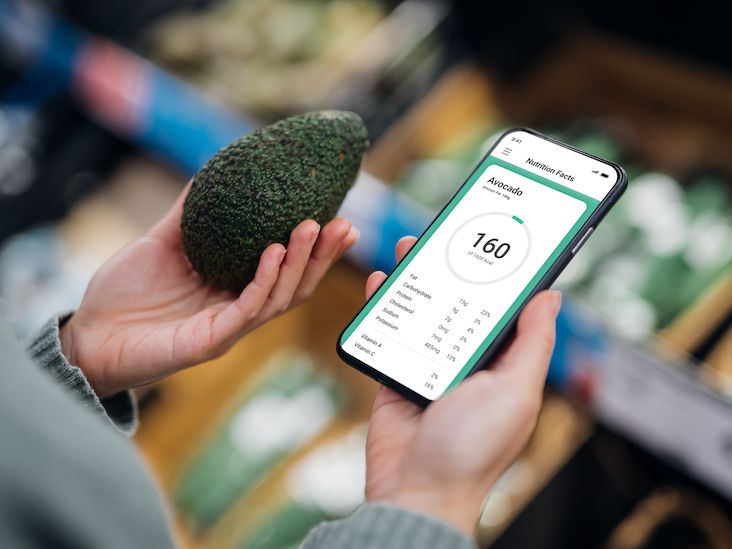
Another powerful tool might already be at your fingertips — your smartphone. You can now control some medical devices directly from smartphone apps.
And if you’re looking for easy ways to track your carbs, insulin doses, A1C levels, blood glucose, glycemic index, blood pressure, or weight, there are many apps for that.
Whether you have type 2 diabetes or you’re cooking for someone with the condition, finding recipes that accommodate your dietary needs can help relieve meal prep frustration and boost mealtime enjoyment in a big way.
Opt for recipes that provide low to moderate amounts of carbs, and plenty of protein, fiber, and healthy fats.
It’s best to work with your doctor or another healthcare professional to initially help you figure out the number of carbohydrates to shoot for in your meals and snacks.
Consider working with a dietitian who’s trained in diabetes. They’ll take your overall health, age, activity level, and other needs into account to help you craft a customized eating plan.




