In-hospital use for COVID-19Actemra (tocilizumab) has been given an emergency use authorization (EUA). This EUA allows for
in-hospital use of Actemra as a treatment for COVID-19 in certain cases. You should not take any prescription drug, including Actemra, unless your doctor recommends that you do so.For information on prevention and treatment, as well as expert tips, visit our COVID-19 hub.
If you have certain conditions that affect your immune system, your doctor might prescribe Actemra for you.
Actemra is a prescription drug that can be used to treat the following conditions:
- rheumatoid arthritis in adults
- giant cell arteritis in adults
- interstitial lung disease (if it’s related to a condition called systemic sclerosis) in adults
- polyarticular juvenile idiopathic arthritis (JIA) in some children
- systemic JIA in some children
- cytokine release syndrome in adults and some children
Actemra may only be recommended for certain people with these conditions. For more information about the specifics of Actemra, see the “What is Actemra used for?” section below.
Actemra basics
Actemra comes as a liquid solution. It can be given as an injection under your skin or as an intravenous (IV) infusion (an injection into your vein given over time). Your doctor will determine whether you should receive Actemra as an injection or an infusion.
Actemra contains the drug tocilizumab, which is a biologic medication. A biologic is made from parts of living organisms. Actemra is not available in a biosimilar form. (Biosimilars are like generic drugs. But unlike generics, which are made for non-biologic drugs, biosimilars are made for biologic drugs.) Instead, tocilizumab is available only as the brand-name drug Actemra.
Like most drugs, Actemra may cause mild or serious side effects. The lists below describe some of the more common side effects that Actemra may cause. These lists don’t include all possible side effects.
Keep in mind that side effects of a drug can depend on:
- your age
- other health conditions you have
- other medications you take
Your doctor or pharmacist can tell you more about the potential side effects of Actemra. They can also suggest ways to help reduce side effects.
Mild side effects
Here’s a short list of some of the mild side effects that Actemra can cause. To learn about other mild side effects, talk with your doctor or pharmacist or read Actemra’s prescribing information.
Mild side effects of Actemra that have been reported include:
- upper respiratory infection, such as the common cold
- swelling of your nose and throat
- injection or infusion side effects, such as rash*
- headache
- high blood pressure
- high cholesterol
- weight gain or weight loss*
Mild side effects of many drugs may go away within a few days to a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Actemra can occur, but they aren’t common. If you have serious side effects from Actemra, call your doctor right away. But if you think you’re having a medical emergency, you should call 911 or your local emergency number.
Serious side effects of Actemra that have been reported include:
- holes or tears in the stomach or intestines
- liver problems
- low levels of platelets (a type of red blood cell) or neutrophils (a type of white blood cell)
- boxed warning: risk of serious infections*
- higher risk of certain cancers
- nervous system disorders, such as multiple sclerosis
- allergic reaction*
* For more information about this side effect, see the “Side effect focus” section below.
Side effect focus
Learn more about some of the side effects Actemra may cause.
Boxed warning
Actemra has a
Actemra may weaken your immune system. Due to this, the medication can increase your risk of developing an infection. Although most infections are mild, it’s possible to develop a serious infection during your Actemra treatment. In rare cases, infections may require treatment in a hospital and may even be life threatening.
In studies, people receiving Actemra who developed a serious infection were usually also taking other drugs that weakened their immune systems. Examples of these medications include methotrexate (Trexall) or steroid medications such as prednisone (Rayos).
Examples of infections that can occur may include:
- tuberculosis (TB)*
- fungal infection, such as yeast infection
- bacterial infection, such as urinary tract infection (UTI)
- viral infection, such as pneumonia
Symptoms of an infection can vary but may include:
- fever
- cough
- chills
- stuffy nose or runny nose
- sore throat
- muscle aches or pains
- unexplained weight loss
* Actemra can reactivate TB (cause TB symptoms) if you’ve had the condition before.
What might help
Before you start treatment with Actemra, your doctor will likely check to make sure that you don’t have any infections. This includes testing you for tuberculosis. If you do have an infection, your doctor will likely recommend treating your infections before you start Actemra treatment.
During your treatment, it’s important that you tell your doctor right away if you develop symptoms of an infection. Treating an infection as soon as possible can help prevent it from becoming severe.
Be sure to tell your doctor if you’ve had infections that keep coming back, have had TB, or have any other conditions that may raise your risk of infection. Your doctor can determine if Actemra may be a safe treatment option for you.
If you develop an infection during your treatment, your doctor will likely pause your treatment until the infection is cleared.
Injection or infusion side effects
Actemra may be given as an injection under the skin or as an intravenous (IV) infusion. (An IV infusion is an injection into your vein given over time.) Some people may experience side effects at the site of the injection. People receiving the drug by IV infusion may have side effects during or shortly after their infusion.
In studies, these side effects were common in people receiving Actemra as an injection under the skin. In comparison, infusion side effects were less common.
Examples of injection or infusion side effects that can occur include:
- redness or discoloration
- itching
- pain
- swelling
In addition, infusion side effects can also include:
- changes in blood pressure
- headache
- dizziness
- nausea
- diarrhea
What might help
If you experience injection side effects during your Actemra treatment, talk with your doctor or pharmacist. They may be able to recommend over-the-counter medications to manage your symptoms. For example, they may recommend acetaminophen (Tylenol) or diphenhydramine (Benadryl) to help prevent injection side effects.
During your Actemra infusion, you’ll likely be monitored for infusion side effects. But keep in mind that side effects can happen up to 24 hours after your infusion ends. It’s important to tell your doctor if you experience any side effects after your infusion.
Weight gain or weight loss
Actemra may cause weight changes in some people. In studies, weight gain was reported in people receiving Actemra for rheumatoid arthritis (RA), but this wasn’t a common side effect.
In the studies, weight gain wasn’t reported in people receiving Actemra for other conditions. So it’s not known if weight gain may occur if you use Actemra for a condition other than RA.
Weight loss was not reported in studies of people taking Actemra. But weight loss can be a symptom of a serious infection. Actemra can raise your risk of developing serious infections, so tell your doctor right away if you notice any unexplained weight loss.
What might help
If you experience changes in weight during your Actemra treatment that concerns you, talk with your doctor. They can determine what may be causing these changes. If you experience weight loss, your doctor may check for other symptoms of an infection.
Allergic reactionSome people may have an allergic reaction to Actemra.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (temporary warmth, redness, or deepening of skin color)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause trouble breathing.
Call your doctor right away if you have an allergic reaction to Actemra. But if you think you’re having a medical emergency, call 911 or your local emergency number.
Costs of prescription drugs can vary depending on many factors. These factors include what your insurance plan covers and which pharmacy you use.
If you have questions about how to pay for your prescription, talk with your doctor or pharmacist. You can also visit the Actemra manufacturer’s website to see if they have support options.
You can check out this article to learn more about saving money on prescriptions.
Below are commonly used dosages, but your doctor will determine the right dosage for you.
Form and strengths
Actemra comes as a liquid solution. It can be given as an injection under your skin or as an intravenous (IV) infusion (an injection into your vein given over time).
Your doctor will recommend whether you should receive Actemra as an injection or an infusion. If you receive Actemra through injection, your doctor may be able to show you or your caregiver how to inject the drug at home. If you receive Actemra through IV infusions, these will be given in either your doctor’s office, a hospital, or an infusion clinic.
For Actemra injections, the drug is available in a prefilled syringe or as a prefilled autoinjector (called ACTPen). Both the pen and prefilled autoinjector contain 162 milligrams (mg) of Actemra in 0.9 milliliters (mL) of solution.
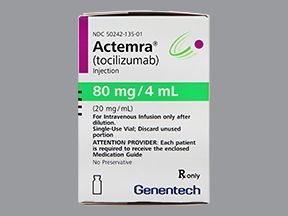
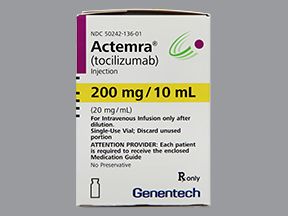
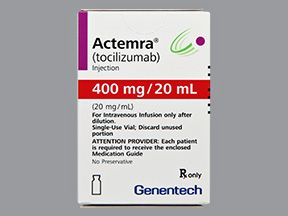
For IV infusions, Actemra comes in vials in the following strengths:
- 80 mg/4 mL
- 200 mg/10 mL
- 400 mg/20 mL
Recommended dosages
Your doctor will determine the best dosage of Actemra for you. They may use a dosing calculator to calculate your Actemra dosage based on your body weight.
If you have rheumatoid arthritis or giant cell arteritis (GCA), you can receive Actemra via either injection or IV infusion. For the injections, you’ll likely take a dose every week or every other week. If you receive IV infusions, you’ll receive a dose every 4 weeks.
For interstitial lung disease, Actemra is only given by injection. You’ll likely take one dose of Actemra per week.
To treat polyarticular juvenile idiopathic arthritis (PJIA) or systemic juvenile idiopathic arthritis (SJIA), Actemra can be given by injection or IV infusion. If you use injections, you’ll take a dose every 2 to 3 weeks for PJIA or every 1 to 2 weeks for SJIA. For IV infusions, Actemra is given every 4 weeks for PJIA or every 2 weeks for SJIA.
For cytokine release syndrome, Actemra is only given through IV infusion. For this condition, you’ll likely receive just one dose of Actemra. But in some cases, your doctor may determine that you need additional doses. This may depend on how severe your condition is and how your body responds to the drug.
Questions about Actemra’s dosage
- What if I miss a dose of Actemra? If you receive Actemra through IV infusion and miss your appointment, call to reschedule your appointment right away. If you administer Actemra injections at home and forget to take your dose, call your doctor to see when you should take your next dose of Actemra. They can help determine the best dosing schedule for you.
- Will I need to use Actemra long term? It depends on the condition you’re using Actemra to treat. For CRS, you may only need one dose. For the other conditions Actemra is used to treat, your doctor may recommend that you take it long term if the drug is working for you.
- How long does Actemra take to work? Actemra begins to work right after you take your first dose of medication. But depending on the condition you’re using Actemra to treat, it may take time before you notice a decrease in your symptoms. It can take up to 14 weeks for Actemra to reach a consistent level in your body. If you have questions about when you should expect to see results from Actemra, talk with your doctor.
Find answers to some commonly asked questions about Actemra.
How does Actemra work? And how long does it stay in your system?
Actemra is used to treat the following conditions:
- rheumatoid arthritis (RA)
- giant cell arteritis
- interstitial lung disease (ILD), if it’s related to a condition called systemic sclerosis
- polyarticular juvenile idiopathic arthritis
- systemic JIA
- cytokine release syndrome
All of these conditions increase inflammation (swelling and damage) in your body. Actemra’s mechanism of action, or the way the drug works, is that it blocks a protein called interleukin-6 (IL-6). IL-6 increases the activity of your immune system, which may cause inflammation.
Actemra works to reduce inflammation caused by your condition, which can help relieve your symptoms.
The amount of time Actemra stays in your body depends on the condition you’re taking Actemra to treat. It may also depend on your body weight and whether you receive Actemra as an injection under your skin or as an intravenous (IV) infusion. (An IV infusion is an injection into your vein given over time.)
Based on the half-life of Actemra, the drug may stay in your system for up to 13 weeks. (The half-life is the amount of time it takes your body to remove half of the drug.) The half-life of Actemra can range from about 4 to 19 days.
It generally takes about five half-lives for a drug to leave your body completely. This means Actemra may stay in your body for about 3 to 13 weeks.
If you have other questions about how Actemra works or how long it may affect you, talk with your doctor or pharmacist.
What is Actemra’s drug class? Is it a TNF inhibitor?
Actemra belongs to a group of drugs called interleukin-6 (IL-6) antagonists. These drugs work by blocking a protein called IL-6, which contributes to inflammation (swelling and damage) in your body.
Actemra is not a tumor necrosis factor (TNF) inhibitor. These drugs block a different protein, called TNF, which may also contribute to inflammation. Examples of TNF inhibitors include:
To find out which type of drug may work best for you, talk with your doctor.
Is Actemra similar to the alternative drug Humira?
Yes, Actemra is similar to Humira in some ways. But these drugs also have many differences.
Actemra and Humira are both used to treat rheumatoid arthritis and some forms of juvenile idiopathic arthritis. But Actemra is also approved to treat:
- giant cell arteritis
- interstitial lung disease, if it’s related to a condition called systemic sclerosis
- cytokine release syndrome
In addition, Humira can be used to treat:
- psoriatic arthritis
- ankylosing spondylitis
- Crohn’s disease
- ulcerative colitis
- plaque psoriasis
- hidradenitis suppurativa
- uveitis
Both Actemra and Humira can be given as an injection under the skin. But Actemra may also be given as an IV infusion.
These medications work in different ways to decrease inflammation in the body. Actemra blocks a protein called IL-6, and Humira blocks a protein called TNF.
Actemra and Humira may also differ in their dosages and side effects. To learn more about how these drugs compare, talk with your doctor. They can determine if one of these drugs may be right for you.
How should I store Actemra?
If you use Actemra at home, store the prefilled syringes or prefilled autoinjectors in the refrigerator at a temperature of 36°F to 46°F (2°C to 8°C). You should not freeze Actemra.
You should also protect Actemra from light. This can be done by keeping it in its original packaging. Do not get the syringe or autoinjector wet.
If you have other questions about how to store Actemra properly, talk with your doctor or pharmacist.
Does Actemra cause hair loss?
No, you shouldn’t experience hair loss during your Actemra treatment. This wasn’t a side effect reported by people receiving Actemra in studies.
But in some cases, your doctor may recommend that you take Actemra along with other medications to treat your condition. These other medications may cause hair loss. For example, some people receiving Actemra also take methotrexate (Trexall), and this drug can cause hair loss.
Also, some of the conditions Actemra is used to treat can cause hair loss. For example, people with rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, or systemic juvenile idiopathic arthritis may experience hair loss from their condition.
If you’re concerned about hair loss during your Actemra treatment, talk with your doctor or pharmacist.
Is Actemra used to treat depression or PMR?
Actemra is not currently approved to treat depression or polymyalgia rheumatica (PMR). But in some cases, your doctor may prescribe Actemra off-label to treat depression or PMR. (Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.)
Actemra has been studied as a treatment for depression. But at this time, study data don’t show that the drug is an effective treatment option for this condition. In fact, one
Other studies have tested the use of tocilizumab in people with PMR. One study showed that tocilizumab may be an effective treatment option for this condition when used along with steroid medications. Prednisone (Rayos) is an example of a steroid that may be used along with Actemra.
If you’re interested in using Actemra for depression or PMR, talk with your doctor about your treatment options.
Actemra is used to treat the following conditions:
- rheumatoid arthritis (RA)
- giant cell arteritis (GCA)
- interstitial lung disease (ILD), if it’s related to a condition called systemic sclerosis
- polyarticular juvenile idiopathic arthritis (PJIA)
- systemic JIA (SJIA)
- cytokine release syndrome (CRS)
All the conditions that Actemra treats are autoimmune conditions that increase inflammation (swelling and damage) in your body. Actemra works by blocking a protein called interleukin-6 (IL-6), which can cause inflammation and increase the activity of your immune system. Actemra reduces the inflammation, which can help relieve your symptoms.
See below for details on Actemra’s use for each condition.
RA
RA occurs when your immune system attacks your joints. Actemra is used in adults with moderate to severe RA who have already tried one or more disease-modifying antirheumatic drugs (DMARDs). Examples of DMARDs include methotrexate (Trexall) or leflunomide (Arava). In some cases, Actemra may be used with methotrexate or other DMARDs to treat RA.
GCA
GCA causes swelling of the arteries that provide blood to the head and brain. If not treated, this condition could affect your vision. Actemra is used to treat GCA in adults.
For GCA, your doctor may prescribe Actemra alone or along with steroid medications, such as prednisone (Rayos).
PJIA and SJIA
PJIA and SJIA are types of arthritis that affect children. With PJIA, the immune system attacks multiple joints. SJIA is arthritis that affects the whole body. Actemra is used in children ages 2 years and older with PJIA or SJIA. Children taking Actemra for these conditions may also take methotrexate along with it.
ILD
Actemra can be used in adults to treat ILD that’s related to systemic sclerosis. ILD is a condition that causes swelling and scarring of the lungs, which can make it harder to breathe. Systemic sclerosis causes hardening of your tissue, which may affect your blood vessels or organs.
Actemra works to treat ILD related to systemic sclerosis by easing symptoms of the condition, such as shortness of breath, chest pain, and cough.
CRS
Actemra can be used to treat severe or life threatening CRS in adults and children ages 2 years and older. This drug can be used if your CRS was caused by a type of cancer treatment called chimeric antigen receptor (CAR) T-cell therapy. Your doctor may prescribe Actemra alone or together with a steroid medication such as prednisone (Rayos).
Actemra can be given as an injection under your skin or as an intravenous (IV) infusion. (An IV infusion is an injection into your vein given over time). Your doctor will recommend whether you should receive Actemra as an injection or an infusion, and they’ll explain how you’ll take or receive the drug.
Using Actemra
If you use the injection form of Actemra, you’ll likely get your first doses in your doctor’s office. After that, your doctor may be able to show you or your caregiver how to inject your dose of Actemra at home. Actemra can be injected into your thigh, your belly, or the outside of your upper arm.
You should rotate your injection sites by using a new area that’s at least 1 inch away from the last area you used. This can help prevent scar tissue from forming. You should also avoid injecting your dose into any moles, bruises, or scars.
For more information on how to inject your dose of Actemra, see the written instructions or instructional video on the manufacturer’s website.
If you receive Actemra through IV infusions, these will be given in either your doctor’s office, a hospital, or an infusion clinic. Actemra infusions typically take about 1 hour.
Accessible medication containers and labels
If it’s hard for you to read the label on your prescription, tell your doctor or pharmacist. Certain pharmacies may provide medication labels that:
- have large print
- use braille
- contain a code you can scan with a smartphone to change the text into audio
Your doctor or pharmacist may be able to recommend a pharmacy that offers these options if your current pharmacy doesn’t.
Using Actemra with other drugs
In some cases, your doctor may prescribe Actemra along with other medications to treat your condition.
For example, people using Actemra for rheumatoid arthritis (RA), polyarticular juvenile idiopathic arthritis, or systemic juvenile idiopathic arthritis may use Actemra with methotrexate (Trexall). Methotrexate is a disease-modifying antirheumatic drug (DMARD).
If you have RA, your doctor may recommend using Actemra with other DMARDs, such as hydroxychloroquine (Plaquenil) or leflunomide (Arava).
If you use Actemra to treat giant cell arteritis or cytokine release syndrome, your doctor may prescribe Actemra along with a steroid medication, such as prednisone (Rayos).
Talk with your doctor about the best treatment plan for you. Based on your condition, they can determine if you should take Actemra alone or with other drugs.
Questions for your doctorYou may have questions about Actemra and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions such as:
- How will Actemra affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, don’t be afraid to ask questions or offer feedback on your treatment.
Before you start treatment with Actemra, it’s important to tell your doctor about any other medical conditions you have and other medications you take. This can help your doctor be sure that Actemra is a safe treatment option for you.
Interactions
Taking a medication with certain vaccines, foods, and other things can affect how the medication works. These effects are called interactions.
Before taking Actemra, be sure to tell your doctor about all medications you take, including prescription and over-the-counter types. Also, describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Actemra.
Interactions with drugs or supplements
Actemra can interact with several types of drugs. These include:
- statin drugs, such as lovastatin (Altoprev), atorvastatin (Lipitor), or simvastatin (Zocor)
- omeprazole (Prilosec), an acid reflux treatment
- the cough medication dextromethorphan (Delsym)
- birth control pills
- warfarin (Jantoven), a blood thinner
- cyclosporine (Neoral), a transplant medication
- the asthma drug theophylline (Theo-24)
This list does not contain all types of drugs that may interact with Actemra. Your doctor or pharmacist can tell you more about these interactions and any others that may occur with the use of Actemra.
Other interactions
Actemra may also interact with live vaccines. (With live vaccines, you receive a weakened form of a virus.) Examples of live vaccines include:
- chickenpox
- measles, mumps, rubella (MMR)
- intranasal flu (FluMist)
Before starting treatment with Actemra, talk with your doctor about any vaccines you may need.
Boxed warning
Actemra has a
Actemra has a boxed warning for the risk of serious infections. An infection can occur because Actemra may weaken your immune system. Although most infections are mild, it’s possible to develop a serious infection during your Actemra treatment. In some cases, infections may require treatment in a hospital and may even be life threatening.
You may have a higher risk of serious infection if you’re also taking other drugs that weaken your immune system. Examples include methotrexate (Trexall) or steroid medications such as prednisone (Rayos).
Tell your doctor if you:
- have a history of infections that keep coming back
- have had tuberculosis
- have any other conditions that may raise your risk of infection
Your doctor can help determine if Actemra may be a safe treatment option for you.
Other warnings
Actemra may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take Actemra. Factors to consider include those in the list below.
- Liver problems. Actemra may raise your risk of liver problems. If you already have liver problems, using Actemra may make them worse. Your doctor may want to monitor your liver function more closely during your Actemra treatment. In some cases, your doctor may prescribe a lower dose of Actemra. Or they may recommend a different treatment option for you.
- Tuberculosis. Before Actemra treatment, tell your doctor if you’ve had tuberculosis (TB) before. Actemra could cause your TB to come back. Your doctor will likely test you for tuberculosis before you start treatment with Actemra. If you have TB, they may recommend treating it before you start taking Actemra.
- Hepatitis B. Before starting your Actemra treatment, tell your doctor if you have hepatitis B or have had it in the past. Actemra may cause your hepatitis B to reactivate (flare up), so your doctor may monitor you more closely during your Actemra treatment.
- Allergic reaction. If you’ve had an allergic reaction to Actemra or any of its ingredients, your doctor will likely not prescribe Actemra. Ask your doctor what other medications are better options for you.
- Stomach problems, such as ulcers or diverticulitis. Actemra could cause holes or tears in the stomach or intestines. If you have other stomach problems, such as diverticulitis or ulcers, you may have a higher risk of developing these side effects. Your doctor can determine if Actemra may be a safe treatment option for you.
- Nervous system conditions, such as multiple sclerosis. Although very rare, it’s possible to develop a nervous system condition such as multiple sclerosis from taking Actemra. If you already have a nervous system condition, Actemra could make it worse. Talk with your doctor to see if Actemra may be a safe treatment option for you.
- Current infections. Before starting treatment with Actemra, talk with your doctor about any infections you have. This drug may weaken your immune system and increase your risk of infection. If you already have an infection, Actemra may make it worse. Your doctor will likely prescribe medication to treat your infection before you start Actemra treatment.
- Recent vaccinations. You should not receive any live vaccines during your Actemra treatment. Examples of live vaccines include those for chickenpox and measles, mumps, and rubella (MMR). Live vaccines contain a weakened form of a virus. Because Actemra can weaken your immune system, your body may not be able to fight the virus in the vaccine. Before starting Actemra, it’s important to tell your doctor about any vaccines you’ve recently received. They can determine when it may be safe to start your Actemra treatment.
Actemra and alcohol
There are no known interactions between Actemra and alcohol. But both Actemra and alcohol can cause liver problems. Drinking large amounts of alcohol during your Actemra treatment may raise your risk of liver problems.
If you drink alcohol, talk with your doctor about how much may be safe for you to drink during your treatment.
Pregnancy and breastfeeding
It’s not known if Actemra is safe to use during pregnancy. Actemra may cause harm to a fetus.
If you do become pregnant during your Actemra treatment, consider enrolling in the drug’s pregnancy registry. A pregnancy registry collects data about the drug’s use during pregnancy. The registry can help show if a drug may cause harm during pregnancy. You can sign up for the registry online or by calling 1-877-311-8972.
It’s also unknown whether Actemra may be safe to use while breastfeeding. This is because it’s not known whether the drug passes into breast milk and, if so, what effects it could have on a breastfed child.
If you’re pregnant or breastfeeding, or planning to become pregnant or breastfeed, talk with your doctor before starting Actemra treatment.
To learn how Actemra and Kevzara compare, see this article. Also, you can talk with your doctor to find out which drug may be right for you.
If you’d like to know more about how Actemra compares with Orencia, check out this article. Your doctor can also tell you more about these treatment options.
Using more than the recommended dosage of Actemra can lead to serious side effects. For example, you could develop low levels of neutrophils (a type of white blood cell), which can raise your risk for infection.
What to do in case you take too much Actemra
Call your doctor if you think you’ve received too much Actemra. You can also call 800-222-1222 to reach the American Association of Poison Control Centers, or use its online resource. However, if you have severe symptoms, immediately call 911 or your local emergency number. Or go to the nearest emergency room.
Before you start your Actemra treatment, talk with your doctor about any questions you may have about the drug. Here are some example questions to help you get started:
- Which form of Actemra is best for me?
- How should I treat side effects that I may experience from this medication?
- What should I do if I become pregnant during my Actemra treatment?
- If Actemra isn’t working for me, can my dose be increased?
To learn more about treatment options for rheumatoid arthritis, see this article about other medications. You can also sign up for the rheumatoid arthritis newsletter here.
For more information about the treatment options available for giant cell arteritis, see this article.
Q:
Could the other medications I’m taking with Actemra increase my risk of side effects?
AnonymousA:
Yes, it’s possible.
Depending on the condition you’re using Actemra to treat, you may take it along with other medications. Examples include methotrexate (Trexall) or steroids such as prednisone (Rayos). These other medications could raise your risk of certain side effects with Actemra.
For example, Actemra may cause serious infections. In studies of Actemra, serious infections occurred in people who were also taking other drugs that affected their immune system activity. This includes medications such as methotrexate and steroids.
Your doctor will determine if you should take Actemra alone or with other drugs. They can also discuss your risk of infections with Actemra. And while you take Actemra, your doctor will monitor you for signs of an infection and other possible side effects.
Editor’s Note: Actemra has a
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.