Key takeaways
- Ozempic is approved by the Food and Drug Administration (FDA) for certain uses in people with type 2 diabetes. It can be prescribed off-label to help with weight loss, but it’s not approved for this use.
- Ozempic is given as a once-weekly injection under the skin, using prefilled disposable pens.
- Savings programs and coupons may be available to help lower the cost of Ozempic injections.
Ozempic can be prescribed for adults with type 2 diabetes to:
- lower certain risks in people who also have heart disease, including heart attack and stroke
- help manage blood sugar levels, along with lifestyle improvements in diet and exercise
- prevent worsening kidney function and heart-related death in people who also have chronic kidney disease (CKD)
To learn more about Ozempic’s approved uses, see the “What is Ozempic used for?” section.
Doctors may also prescribe Ozempic off-label for weight loss or weight management. (With off-label use, a drug that’s approved for certain conditions is prescribed for another purpose.) However, the drug is not approved by the FDA for this purpose.
Ozempic basics
Ozempic contains the active ingredient semaglutide. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists.
Ozempic is a brand-name medication that’s not currently available in generic form.
Ozempic has a boxed warning. A boxed warning is the most serious warning from the FDA. For details, see the “What should be considered before taking Ozempic?” section.
Ozempic is FDA approved to:
- Help manage blood sugar levels in adults with type 2 diabetes, along with lifestyle improvements in diet and exercise.
- Lower the risk of certain heart or blood vessel problems in adults who have both heart disease and diabetes. These risks can include heart attack, stroke, and death due to heart or blood vessel issues.
- Lower the risk of kidney disease progression and heart-related death in adults with diabetes and CKD.
With diabetes, you have elevated blood sugar levels. Over time, this can damage blood vessels in your body.
Ozempic helps lower blood sugar levels and reduce the risk of certain heart and blood vessel problems.
Note: There are some limitations to how Ozempic can be used. These are as follows:
- This drug hasn’t been studied in people who have had pancreatitis in the past. (With pancreatitis, you have inflammation in your pancreas.) Other treatments should be considered if you’ve had this condition.
- Ozempic isn’t meant to treat type 1 diabetes or diabetic ketoacidosis (DKA). (DKA is a dangerous condition that occurs when you have a high level of acidic substances called ketones in your body.)
Doctors might prescribe Ozempic off-label for weight loss. (With off-label use, a drug that’s approved for certain conditions is prescribed for another purpose.) However, the drug is not approved by the FDA for this purpose. (For more information, see the section of this article called “Is Ozempic used for weight loss?”)
Ozempic works in several ways to lower blood sugar levels in people with type 2 diabetes. The drug also lowers heart-related risks in people with both diabetes and heart disease.
The drug does this in the following ways:
- Ozempic mimics the actions of a naturally produced hormone called GLP-1. By activating GLP-1 receptors in your brain, Ozempic helps stimulate the pancreas to release insulin.
- Similar to the GLP-1 hormone, Ozempic slows the movement of food through your stomach. This causes you to feel full for longer periods of time. In turn, it prevents a big increase in your blood sugar levels and can lead to fewer hunger cravings.
- It increases the amount of insulin your body makes after a meal so that your blood sugar levels won’t get too high. Insulin is a hormone that lowers your blood sugar levels.
- It lowers the amount of sugar released into your bloodstream.
Your doctor or a pharmacist can provide details about how Ozempic works in the body.
Whether you have health insurance or not, cost may be a factor when you’re considering Ozempic. What you’ll pay for Ozempic may depend on several things, such as your treatment plan and the pharmacy you use.
Here are a few things to consider regarding cost:
- Drug coupons: You may be able to find drug coupons on prescription discount websites that can reduce the cost of your medication. These coupons cannot be used with insurance copays or benefits, but the discounted price may be lower than what you would pay through insurance.
- Savings program: Savings programs may be available to help reduce Ozempic’s price. If you have questions about how to pay for your prescription, talk with your doctor or pharmacist.
You can refer to this article for details about the cost of Ozempic. You can also check out this article to learn more about saving money on prescriptions.
Like most drugs, Ozempic may cause mild or serious side effects. The following lists describe some of the more common side effects reported with Ozempic. These lists don’t include all possible side effects.
Your doctor or pharmacist can tell you more about the potential side effects of Ozempic. They can also suggest ways to help reduce side effects. For more details, see this article about Ozempic’s side effects.
Mild side effects
Here’s a short list of some of the mild side effects reported with Ozempic. To learn about other mild side effects, talk with your doctor or pharmacist or read Ozempic’s prescribing information.
Mild side effects of Ozempic can include:
- constipation
- diarrhea
- abdominal pain
- vomiting
- nausea (see “Side effect focus” for details)
Mild side effects of many drugs may go away within a few days or a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Ozempic can occur, but they aren’t common. If you have serious side effects from Ozempic, call your doctor right away. But if you think you’re having a medical emergency, you should call 911 or your local emergency number.
Serious side effects can include:
- diabetic retinopathy (damage to your eyes that’s caused by diabetes)
- hypoglycemia (low blood sugar)
- gallbladder disease (which can include gallstones and inflammation of your gallbladder)
- nausea*
- pancreatitis*
- boxed warning: risk of thyroid tumors or thyroid cancer?
* For more information, see the “Side effect focus” section.
? For more information, see the “What should be considered before taking Ozempic?” section.
Side effect focus
Learn more about some of the side effects Ozempic may cause.
Boxed warning
Ozempic has a boxed warning, which is the most serious type of warning from the FDA.
Ozempic has been shown to cause thyroid tumors and thyroid cancer in animals. It is not known whether Ozempic can cause thyroid tumors or medullary thyroid cancer in humans.
If you have a family or personal history of medullary thyroid cancer or a rare endocrine condition called multiple endocrine neoplasia syndrome type 2, you should not take Ozempic.
Talk with your doctor if you have either of these conditions or a family history of them.
What might help
Be sure to call your doctor immediately if you have any signs or symptoms of a thyroid tumor while using Ozempic. These include:
- a lump on your neck
- long-lasting hoarseness in your voice
- shortness of breath
- trouble swallowing
Nausea
Ozempic can cause nausea, especially when you first start taking the medication or when your dose changes. Usually, nausea should go away after a few days.
But keep in mind that nausea can also be a symptom of pancreatitis (inflammation in your pancreas). Pancreatitis is a serious side effect of Ozempic.
If you have nausea that doesn’t go away after a few days, worsens, or becomes severe, call your doctor right away.
What might help
If you have nausea while using Ozempic, your doctor may suggest ways to help manage your symptoms. These may include taking over-the-counter or prescription medications until your nausea gets better. Be sure to check with your doctor before taking any medications for nausea with Ozempic.
Pancreatitis
Ozempic may cause pancreatitis (inflammation of the pancreas). This is a serious condition.
Call your doctor right away if you have any symptoms of pancreatitis. These may include:
- pain, tenderness, or swelling in your upper abdomen
- nausea
- vomiting
Doctors typically won’t prescribe Ozempic if you’ve had pancreatitis in the past.
What might help
If needed, your doctor can order tests to determine whether you have pancreatitis. If necessary, they’ll stop your Ozempic treatment and discuss changes to your treatment plan.
Allergic reaction
For some people, Ozempic can cause an allergic reaction.
This side effect wasn’t reported in the drug’s studies, but it’s been reported since Ozempic was approved for use.
In general, symptoms of allergic reaction can be mild or serious.
What might help?
If you have mild symptoms of an allergic reaction, such as a mild rash, call your doctor right away. They may suggest a treatment to manage your symptoms and can determine whether you should keep taking Ozempic.
If you have symptoms of a severe allergic reaction, such as swelling or trouble breathing, call 911 or your local emergency number right away. These symptoms could be life threatening and require immediate medical care.
If your doctor confirms you’ve had a serious allergic reaction to Ozempic, they may have you switch to a different treatment.
Your doctor will recommend the dosage of Ozempic that’s right for you. The following are commonly used dosages, but always take the dosage your doctor prescribes.
Form and strengths
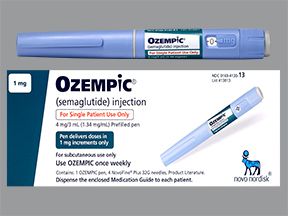
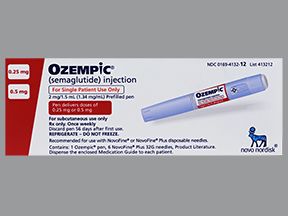
Ozempic comes as a liquid solution inside prefilled, disposable pens. The following table shows which strengths Ozempic pens come in. The strengths are written as milligrams of semaglutide (Ozempic’s active drug) per milliliter of solution (mg/mL).
| Strength | Dose given per injection |
|---|---|
| 2 mg/3 mL (0.68 mg/mL) | 0.25 mg or 0.5 mg |
| 4 mg/3 mL (1.34 mg/mL) | 1 mg |
| 8 mg/3 mL (2.68 mg/mL) | 2 mg |
Your specific dosage may depend on several factors, including:
- the condition you’re using Ozempic to treat
- whether or not you experience any side effects from Ozempic
- any other health conditions you may have
- other medications you may take
For more details about your dosage, talk with your doctor or pharmacist. You can also take a look at this Ozempic dosing guide.
How often do you take Ozempic?
You’ll inject Ozempic once each week. You should use the medication on the same day each week. And try to inject it at about the same time on each of those days.
Your doctor may start you on a low dose of Ozempic for the first 4 weeks of treatment. This way, they can see how well Ozempic is working for you. After this, your doctor will likely increase your dose. Your adjusted dose will depend on your blood sugar levels and other factors.
Each Ozempic pen holds several doses of the drug. Your doctor or pharmacist will explain when you need to throw away each pen and start using a new one.
Questions about Ozempic’s dosage
Here are some common questions about Ozempic’s dosage.
What if I miss a dose of Ozempic?
If you miss a dose of Ozempic, inject the drug as soon as you remember. But only do this if it’s within 5 days of your last dose. If it’s been more than 5 days, skip the missed dose and wait until it’s time for your next scheduled dose. Taking two doses too close together could lead to dangerously low blood sugar levels.
If you miss a dose, check your blood sugar levels regularly to make sure they’re within the standard range. You might find a reminder app useful for staying on track with your weekly injections.
Will I need to use Ozempic long term?
If Ozempic works well for your condition, your doctor may have you take the medication long term. Ask your doctor about the benefits and risks of using Ozempic long term, including its side effects.
How long does Ozempic take to work?
Ozempic starts to work 1 to 3 days after it’s been injected. After you start treatment with Ozempic, it may take 4 to 8 weeks to notice a difference and feel the full benefit.
After at least 4 weeks at your current Ozempic dose, your doctor may increase your dose by up to 1 mg. Your dosage adjustment will depend on your current dosage and how well it’s working for you. It’s important to follow your doctor’s advice on the dose of Ozempic you should take and take it exactly as directed.
Your doctor will explain how to use Ozempic. They’ll also explain how much to take and how often to inject it. Be sure to follow your doctor’s instructions.
Taking Ozempic
Ozempic comes as a liquid solution inside prefilled, disposable pens.
You’ll be able to inject doses of Ozempic yourself. Your doctor or pharmacist can show you how to do this when you first start treatment.
Ozempic injections are given under the skin in your thigh, abdomen, or upper arm. Be sure to rotate the injection site each time you take the medication. You should also use a new needle for each injection. This will help you avoid infections.
Ask your doctor for suggestions to help you feel comfortable and confident managing your injections. Be sure to follow their instructions.
This list contains a few tips you should follow:
- Wash your hands with soap and water before starting.
- Have all your supplies ready, including your Ozempic dose.
- Change the needle every time you use the Ozempic pen.
- Check the pen to make sure that the medication inside is clear and colorless.
- Double-check that the dose is correct on your pen before giving your injection.
- Keep track of your doses and make sure you have a full dose left in your pen after each injection.
- Do not share your pen with anyone else.
- Record the date that your Ozempic prefilled pens should be discarded. (They expire 56 days after opening.)
For instructions on how to use Ozempic, see the manufacturer’s site. Or ask your doctor or pharmacist to show you how to use Ozempic pens.
Taking Ozempic with other drugs
Your doctor may prescribe Ozempic with other medications to help manage your blood sugar levels or lower your risk of cardiovascular problems.
Other diabetes medications that may be prescribed with Ozempic include metformin (Glumetza, Riomet) and empagliflozin (Jardiance).
If you’d like to know more about taking other drugs with Ozempic, talk with your doctor.
Note: For information about things that can interact with Ozempic, such as other drugs or foods, see the “What should be considered before taking Ozempic?” section.
How long do you take Ozempic?
Ozempic can be taken long term. If you and your doctor agree that Ozempic is safe for you, you’ll take it for as long as it continues to be effective for your condition.
Questions for your doctorYou may have questions about Ozempic and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions like:
- How will Ozempic affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
- If you’re new to self-injections, ask your doctor to explain the process to you slowly so that you can follow the steps. Until you’re used to it, don’t worry about asking your doctor to show you the process again.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, don’t be afraid to ask questions or offer feedback on your treatment.
Here’s how Ozempic compares to other medications that have similar uses.
Ozempic vs. Saxenda
You may wonder how Ozempic compares to Saxenda. They both belong to a group of medications called GLP-1 receptor agonists. They have related uses and side effects, but they also have important differences. They each contain different active drugs: Ozempic contains semaglutide, and Saxenda contains liraglutide.
What are their uses?
Ozempic is used to help manage blood sugar levels in people with type 2 diabetes. It is also used to help lower the risk of certain heart or blood vessel problems in adults who have both heart disease and type 2 diabetes.
Saxenda, on the other hand, is a weight management medication. It’s used by people who have obesity or other weight-related conditions, such as high cholesterol, high blood pressure, or type 2 diabetes. Certain children can also take Saxenda.
What are their forms?
Ozempic comes in self-injection pens that are used once weekly. Saxenda also comes in self-injection pens, but it’s injected once daily.
What are their side effects?
Ozempic and Saxenda have some of the same side effects. These include diarrhea, nausea, kidney damage, fatigue (low energy), pancreatitis, and gallbladder disease.
Ozempic and Saxenda can also cause serious side effects, and they both have a boxed warning about a possible risk of thyroid cancer. (A boxed warning is the most serious warning for a drug.)
Talk with your doctor if you have more questions about Ozempic and Saxenda.
How effective are they?
Both Ozempic and Saxenda have been found effective for their approved uses. You can see the prescribing information for Ozempic and Saxenda for details about how each drug performed in studies. You can also talk with your doctor or a pharmacist to learn more about how they compare.
Ozempic vs. Trulicity
You might also like to know how Ozempic compares with Trulicity (dulaglutide). Both drugs belong to a group of medications called GLP-1 receptor agonists. They have similar uses, side effects, and effectiveness, but they contain different active drugs. Ozempic’s active drug is semaglutide, and Trulicity’s active drug is dulaglutide.
What are their uses?
Ozempic and Trulicity are both used to treat type 2 diabetes. Both drugs also have protective effects on the heart and kidneys. The American Diabetes Association (ADA) guidelines recommend their use in people with type 2 diabetes who also have heart disease, heart failure, or kidney disease.
What are their forms?
Both Ozempic and Trulicity come in self-injection pens that you’ll use once weekly.
What are their side effects?
These drugs share some side effects. These include diarrhea, nausea, kidney damage, fatigue, pancreatitis, and diabetic retinopathy. But they also have some unique side effects, such as headache with Ozempic and loss of appetite with Trulicity.
Ozempic and Trulicity have serious side effects, and they both have a boxed warning about a possible risk of thyroid cancer. (A boxed warning is the most serious warning for a drug.)
How effective are they?
Your doctor can provide more information about these medications and determine which one may be most suitable for you.
You can see the prescribing information for Ozempic and Trulicity for more information about how each drug performed in studies. You can also see this detailed comparison of the two drugs.
Talk with your doctor if you have more questions about Ozempic and Trulicity. They can determine which one may suit you best.
Ozempic vs. Victoza
Ozempic and Victoza are both approved to:
- help manage blood sugar levels in adults with type 2 diabetes
- lower risk of serious cardiovascular (heart or blood vessel) problems in adults with type 2 diabetes and heart disease
Victoza can also be used to help manage blood sugar levels associated with type 2 diabetes in children ages 10 years and older.
For more information, see this article on how Ozempic and Victoza compare. You can also talk with your doctor or pharmacist.
Ozempic vs. Wegovy
Ozempic and Wegovy have the same active ingredient, semaglutide. (An active ingredient is what makes a drug work.)
But Ozempic and Wegovy have different approved uses. Ozempic is approved to:
- help manage blood sugar levels in adults with type 2 diabetes
- lower risk of serious cardiovascular (heart or blood vessel) problems in adults with type 2 diabetes and heart disease
Wegovy is approved for long-term weight management, along with lifestyle improvements in diet and exercise. Ozempic is not approved by the FDA for this purpose.
For more information, you can refer to this detailed comparison of Ozempic and Wegovy. You can also talk with your doctor or pharmacist.
Ozempic is not approved by the FDA for use as a weight management medication. But you might lose weight while you’re taking Ozempic. That’s because the medication decreases your appetite.
In some cases, Ozempic is prescribed off-label for weight management, though this isn’t likely. (With off-label use, a drug that’s approved for certain conditions is prescribed for another purpose.) It’s more likely that your doctor would prescribe Wegovy, which contains the same active ingredient as Ozempic, called semaglutide. (An active ingredient is what makes a drug work.) Wegovy is FDA approved to be prescribed for weight management.
Insurance may not cover off-label uses of Ozempic. Ask your doctor for more information.
If you’re interested in using semaglutide for weight management, talk with your doctor. They can help determine the best medication for you and whether it’s appropriate to prescribe Ozempic off-label.
How Ozempic may lead to weight loss
Ozempic may lead to weight loss because:
- It slows down how quickly your stomach empties after eating. This slows your digestion process and can help you feel fuller for longer.
- The drug mimics a hormone called GLP-1 that your body naturally produces. This hormone increases feelings of satiety (feeling full or satisfied after eating).
These effects can also decrease your appetite. For details about how Ozempic works, you can refer to the “How does Ozempic work?” section.
Is Ozempic safe and effective for weight loss? How much weight could I lose with Ozempic?
As long as you use Ozempic as your doctor prescribes, it should be safe for weight loss. However, the drug is not approved by the FDA for this purpose.
The amount of weight you might lose during Ozempic treatment depends on various factors, including how long you use Ozempic and your diet and exercise routine. It also depends on how your body responds to the drug.
For more information about Ozempic’s effectiveness for weight loss, talk with your doctor. They can discuss Ozempic’s studies in more detail and how your lifestyle might affect your weight management treatment. You can also check out this article about how Ozempic is used for weight loss.
How to buy Ozempic
If you think Ozempic could be a good option for you, talk with your doctor. They can help determine whether Ozempic might be right for you and provide a prescription.
There are various ways to get Ozempic. An easy way to purchase Ozempic is by using a telemedicine provider such as:
- Calibrate
- PlushCare
- Ro
- Sesame
Through these services, a licensed telehealth professional will give you a health evaluation. If the evaluation shows that Ozempic could be a helpful option for you, the telehealth professional can provide an electronic prescription. (In some cases, they might refer you to your doctor first.) You can then use this prescription to order the medication through the service’s site. You might be able to pick up your prescription at a nearby pharmacy or have it mailed to you.
After you start taking the medication, the service will provide coaching and other support.
If you get an Ozempic prescription through one of these services, be sure to tell your doctor. It’s important that your doctor knows about all medications you take.
Before starting Ozempic, talk with your doctor about all the benefits and risks of using it. You should also discuss your overall health and any health conditions you may have.
Ask your doctor if Ozempic is safe for you to take if you:
- have a family history of thyroid cancer
- have problems with your pancreas
- have problems with your kidneys
- have diabetic retinopathy (damage to your eyes that’s caused by diabetes)
- are pregnant or plan to become pregnant
- are breastfeeding
Interactions
Using medications, vaccines, foods, and other things with a certain drug can affect how the drug works. These effects are called interactions.
Interactions can raise or lower the effect of medications taken together.
Before taking Ozempic, be sure to tell your doctor about all medications you take (including prescription and over-the-counter types). Also, describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Ozempic.
In addition to the following information, you can also refer to this article on Ozempic’s interactions for more details.
Interactions with drugs or supplements
Ozempic can interact with several types of drugs. This list does not contain all types of drugs that may interact with Ozempic. Your doctor or pharmacist can tell you more about these interactions and any others that may occur while using Ozempic.
If you take Ozempic with other diabetes medications that also lower blood sugar levels, your blood sugar levels might drop too low. This can be dangerous.
Some diabetes medications can increase your insulin levels if taken with Ozempic. In turn, this can lead to low blood sugar. These medications include:
- glimepiride (Amaryl)
- glipizide (Glucotrol XL)
- glyburide (Diabeta, Glynase PresTabs)
- insulin degludec (Tresiba)
- insulin glargine (Lantus, Toujeo)
Note: It’s important to regularly monitor your sugar levels according to your doctor’s advice. Doing so will help you recognize when your blood sugar levels are high (hyperglycemia) or low (hypoglycemia). Talk with your doctor about what to do if your blood sugar levels are either too high or too low.
Foods to avoid with Ozempic
You don’t need to avoid any particular foods while you’re using Ozempic. There aren’t any foods that are known to interact with this drug. And Ozempic doses can be taken with or without food.
Other interactions
Certain herbs and other natural supplements can interact with Ozempic and cause your blood sugar levels to drop. Some examples include:
- bitter melon
- chromium
- gymnema
If you’re taking any herbs or supplements, talk with your doctor about whether they’re safe to take with Ozempic.
Ozempic and alcohol
You should avoid drinking large amounts of alcohol with Ozempic. Large amounts of alcohol can affect your blood sugar level. This can also:
- affect your liver function
- cause dehydration
If you drink alcohol, ask your doctor for more information about the risks of drinking alcohol while you’re taking Ozempic.
Pregnancy and breastfeeding
If you can become pregnant or are breastfeeding, it’s important to consider whether Ozempic is a safe choice for you.
You can refer to this article on Ozempic reproductive health for more information. If you have other questions, talk with your doctor.
Boxed warning
Ozempic has a boxed warning for the risk of thyroid cancer. A boxed warning is the most serious warning from the FDA about drug effects that may be dangerous.
Ozempic has been shown to cause thyroid tumors and thyroid cancer in animals. It is not known whether Ozempic can cause thyroid tumors or medullary thyroid cancer in humans.
If you have a family or personal history of medullary thyroid cancer or a rare endocrine condition called multiple endocrine neoplasia syndrome type 2, you should not take Ozempic.
Talk with your doctor if you have either of these conditions or a family history of them. Be sure to call your doctor immediately if you have any signs or symptoms of a thyroid tumor while taking Ozempic.
Symptoms of a thyroid tumor include:
- a lump on your neck
- long-lasting hoarseness in your voice
- shortness of breath
- trouble swallowing
Other warnings
Ozempic may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take Ozempic. Factors to consider include:
- Kidney damage: Ozempic may cause severe dehydration as a complication of nausea, vomiting, and diarrhea during treatment. In some cases, this dehydration may lead to acute kidney damage. During treatment with Ozempic, be sure to tell your doctor about any digestive side effects you experience. Your doctor will monitor your condition for signs of dehydration or kidney injury, especially after any dosage changes.
- Pancreas disease: Ozempic can cause pancreatitis. If you have pancreas disease or a history of pancreas problems, be sure to discuss this with your doctor. Ozempic has not been studied in people with pancreas disease. Your doctor can help determine whether Ozempic treatment is right for you.
- Gallbladder disease: Ozempic can cause gallbladder problems, including gallstones or inflammation of the gallbladder. If you have a history of gallbladder problems, be sure to talk with your doctor before starting Ozempic treatment. Symptoms of a gallbladder problem include upper abdominal pain, fever, jaundice, and clay-colored stool.
- Diabetes-related eye problems: If you’ve had diabetic retinopathy in the past, Ozempic may worsen this condition. Be sure to talk about this with your doctor before starting Ozempic treatment.
- Allergic reaction: If you’ve had an allergic reaction to Ozempic or any of its ingredients, your doctor will not prescribe Ozempic for you. Ask your doctor about which other medications are better options for you.
- Taking Ozempic with insulin or insulin-increasing drugs: If you’re taking Ozempic along with insulin or drugs that increase how much insulin your body makes, your risk of hypoglycemia increases. (See “Interactions with drugs or supplements” for examples.) Hypoglycemia can be severe. Before you start Ozempic treatment, talk with your doctor about all of the medications you take. If you develop signs of hypoglycemia after using Ozempic (such as headache, drowsiness, or hunger), talk with your doctor. They may adjust the doses of the other drugs you’re taking.
- Slow digestion: Ozempic and diabetes can both cause a digestive problem known as gastroparesis (delayed stomach emptying). This condition slows the movement of food through your digestive system. If you already have gastroparesis, using Ozempic may increase the risk of serious complications from the condition. Your doctor may not prescribe Ozempic if you have a history of severe gastroparesis.
- General anesthesia and deep sedation: Be sure to tell your doctor if you have an upcoming medical procedure that requires general anesthesia or deep sedation. There have been reports of aspiration in people who were sedated during treatment with Ozempic or similar drugs. This is because Ozempic slows down your digestion, causing food to stay in your stomach for longer. Due to the risk of aspiration, you may need to fast for longer than usual before a planned surgery.
Do not take more Ozempic than your doctor prescribes. Doing so can lead to serious side effects.
Because Ozempic is injected once weekly, the effects of an overdose may last for a while. If you take too much Ozempic, your doctor will need to monitor you closely and treat your symptoms until they’ve resolved.
Symptoms of overdose
Ozempic overdose can cause:
- Severe low blood sugar levels (also known as diabetic shock or hypoglycemic shock). Symptoms include:
- dizziness
- feeling jittery
- mood changes
- weakness
- headache
- shakiness
- Severe nausea.
- Severe vomiting.
What to do in case you take too much Ozempic
Call your doctor if you think you’ve taken too much Ozempic. You can also call 800-222-1222 to reach America’s Poison Centers, or you can use its online resource. But if you have severe symptoms, immediately call 911 (or your local emergency number) or go to the nearest emergency room.
There are many treatment options for managing type 2 diabetes. Your doctor can discuss the medications available, including Ozempic. There are several options available for people with heart disease.
You may have questions before taking Ozempic. Be sure to ask your doctor what to expect with treatment. Here are a few questions to consider:
- Is Ozempic available as a pill?
- What lifestyle changes will help my condition?
- How long will it take before Ozempic helps manage my blood sugar levels?
To learn more about Ozempic, see these articles:
- All About Ozempic’s Dosage
- How Much Does Ozempic Cost?
- Ozempic Interactions: Alcohol, Medications, and Others
- Ozempic vs. Trulicity: What You Should Know
- Ozempic vs. Victoza: Which Is Better for Me?
- Side Effects of Ozempic: Examples and Treatment Options
To get information on different conditions and tips for improving your health, subscribe to any of Healthline’s newsletters. You may also want to check out the online communities at Bezzy. It’s a place where people with certain conditions can find support and connect with others.
Q:
What should I do if I remove my Ozempic pen from my skin before the full dose is given?
AnonymousA:
If you remove the Ozempic pen from your skin too soon, you may see a stream of Ozempic coming from the needle tip.
If this happens, you won’t receive the full dose, and you won’t know for sure how much of the drug was injected.
To prevent overdose, do not inject any additional Ozempic. Instead, call your doctor right away. They’ll recommend that you closely monitor your blood sugar levels. And be sure to ask your doctor for guidance about when to give your next injection. They can also let you know how much Ozempic to take at that time.
The Healthline Pharmacist TeamAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.