Stelara (ustekinumab) is a prescription drug used to treat autoimmune conditions such as plaque psoriasis. Stelara comes as a liquid solution given as an injection under the skin or an intravenous (IV) infusion.
Stelara is used to treat:
- plaque psoriasis in adults and some children
- psoriatic arthritis in adults and some children
- Crohn’s disease in adults
- ulcerative colitis in adults
To learn more about these conditions and how Stelara is used for them, see the “What is Stelara used for?” section below.
Stelara basics
Stelara contains the drug ustekinumab, which is a biologic medication. A biologic medication is made from living cells. Ustekinumab also comes in a biosimilar form called Selarsdi (ustekinumab-aekn).* (Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs.)
* The reason “-aekn” appears at the end of the drug’s name is to show that the drug is distinct from similar medications that may be created in the future.
Like most drugs, Stelara may cause mild or serious side effects. The lists below describe some of the more common side effects that Stelara may cause. These lists don’t include all possible side effects.
Your doctor or pharmacist can tell you more about the potential side effects of Stelara. They can also suggest ways to help reduce side effects.
Mild side effects
Here’s a short list of some of the mild side effects that Stelara can cause. Keep in mind that side effects of Stelara might differ slightly depending on the reason you’re using the drug.
To learn about other mild side effects, talk with your doctor or pharmacist, or read Stelara’s medication guide.
Mild side effects of Stelara can include:
- upper respiratory infections, such as the common cold*
- headache
- fatigue (lack of energy)
- abdominal pain
- nausea
- vomiting
- diarrhea
- itchiness
- redness or discoloration at the drug’s injection site
- vaginal yeast infection
- urinary tract infection (UTI)
Mild side effects of many drugs may go away within a few days or a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist.
* For more information about colds, see the “Side effect focus” section directly below.
Serious side effects
Serious side effects from Stelara can occur, but they aren’t common. If you have serious side effects from Stelara, call your doctor right away. However, if you think you’re having a medical emergency, you should call 911 or your local emergency number.
Serious side effects can include:
- posterior reversible encephalopathy syndrome (PRES), which is a condition that causes swelling in your brain and may lead to headache*
- cancer*
- allergic reaction*
- serious infections such as pneumonia (for more information, see the “What should be considered before taking Stelara?” section below)
* For more information about this side effect, see the “Side effect focus” section directly below.
Side effect focus
Learn more about some of the side effects Stelara may cause. For more details about side effects of Stelara, see this article.
Colds
You’re more likely than usual to get a cold when you’re using Stelara. This drug slows down the activity of your immune system, reducing your ability to fight off infections. With lowered immunity, you have a higher risk of catching a cold.
The common cold is an infection caused by viruses. With a cold, you may have symptoms such as:
- cough
- sore throat
- runny nose
- blocked sinuses
- headache
- mild fever
- pain in your sinuses (area around your nose and eyes)
- sneezing
- muscle aches
What might help
If you’re getting colds while you’re taking Stelara, talk with your doctor about ways to help prevent them.
Viruses that cause the common cold are spread between people through the air and on surfaces. To help reduce your risk of catching a cold, try the following tips:
- wash your hands frequently with soap and water
- avoid touching your face with unwashed hands
- avoid contact with or stay physically distanced from people who are sick
You may also want to use over-the-counter (OTC) medications to treat your cold symptoms. But be sure to check with your doctor or pharmacist before using any medications with Stelara. Keep in mind that some OTC medications may help relieve cold symptoms. But the medications won’t cure your cold. You can also talk with your doctor or pharmacist about other remedies for your cold symptoms.
Headaches
You may have headaches while you’re taking Stelara. This is one of the most common side effects of the drug.
While using Stelara, you may also have headaches from a condition called posterior reversible encephalopathy syndrome (PRES). PRES is a rare but serious condition that’s due to swelling in the brain. It was seen in studies of people taking Stelara.
Other symptoms you may have with PRES include:
- seizures
- confusion
- changes in your vision
It’s possible to develop symptoms of PRES after a few days to a few months of starting Stelara.
What might help
If you have headaches when using Stelara, talk with your doctor. But seek emergency medical attention if you have a headache along with other symptoms of PRES.
If you have PRES, your doctor will have you stop taking Stelara. But don’t stop taking Stelara without talking with your doctor.
Keep in mind that having headaches while using Stelara doesn’t always mean you have PRES. Several OTC drugs can help relieve the discomfort of a headache. Check with your doctor or pharmacist about which options are safe for you.
Cancer
Stelara lowers the activity of your immune system. And this may increase your risk for certain cancers. In studies, some people taking Stelara were more likely to get skin cancer.
Before starting Stelara, tell your doctor if you’ve ever had cancer. This drug wasn’t studied for safety in people with a history of cancer.
What might help
While you’re taking Stelara, your doctor will monitor you for any signs of skin cancer.
You may have a higher risk for cancer and need closer monitoring during treatment if you:
- are ages 60 years or older
- have taken drugs that work on your immune system over a long period of time
- used photochemotherapy (PUVA) treatment in the past
While taking Stelara, check your skin regularly for any changes. Be sure to tell your doctor if you notice any new growths or other changes. If you’d like, ask your doctor to show you how to do your own skin exam.
Allergic reactionSome people may have an allergic reaction to Stelara. In addition, if you’re allergic to latex, you shouldn’t handle the needle cover of Stelara’s prefilled syringe. It contains latex and may cause an allergic reaction if you’re sensitive to latex.
Symptoms of a mild allergic reaction can include:
- rash
- itchiness
- flushing (warmth, swelling, redness, or discoloration in your skin)
A more severe allergic reaction is rare but possible. Severe allergic reactions were seen in people during studies of Stelara. If you have a severe allergic reaction, you must seek medical help right away and stop using Stelara.
Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause trouble breathing.
Call your doctor right away if you have an allergic reaction to Stelara. But if you think you’re having a medical emergency, call 911 or your local emergency number.
Your doctor will recommend the dosage of Stelara that’s right for you. Below are commonly used dosages, but always inject the dosage your doctor prescribes.
Forms and strengths
Stelara comes as a liquid solution inside prefilled syringes and single-dose vials. You’ll receive this solution as an injection under your skin.
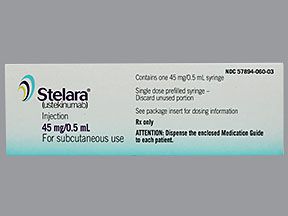
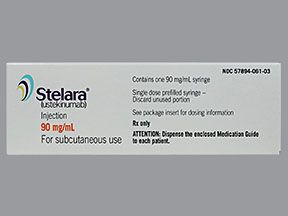
Stelara liquid solution for injection under your skin is available in two strengths:
- 90 milligrams/milliliter (mg/mL), in single-dose prefilled syringes
- 45 mg/0.5 mL, in single-dose prefilled syringes and single-dose vials
Stelara also comes as a solution inside single-dose vials that you’ll receive from healthcare professionals as an intravenous (IV) infusion. With an IV infusion, you’ll get the medication through your vein over a period of time.
Stelara liquid solution for IV infusion is available in single-dose vials in one strength: 130 mg/26 mL.
Recommended dosages
Your doctor will recommend the dosage of Stelara that’s right for you. Below are commonly used dosages, but the dosage you receive will be determined by your doctor.
Dosage for Crohn’s disease or ulcerative colitis
If you have Crohn’s disease or ulcerative colitis, your doctor may prescribe either an IV infusion or an injection of Stelara. In some cases, your doctor may prescribe a loading dose of the drug. (A loading dose is a one-time dose that’s given to boost your body’s level of a drug.) For a loading dose, you’ll receive the drug as an IV infusion that will last at least 1 hour.
After the IV infusion, your doctor will prescribe injections of Stelara. You’ll receive Stelara as an injection under your skin 8 weeks after you took the loading dose. Then, you’ll keep getting these injections once every 8 weeks.
Dosage for plaque psoriasis or psoriatic arthritis
If you’re an adult with plaque psoriasis or psoriatic arthritis, you’ll receive one dose of Stelara followed by another dose 4 weeks later. After the second dose, you’ll receive a Stelara injection once every 12 weeks.
Children with plaque psoriasis or psoriatic arthritis who are ages 6 to 17 years old will follow the adult dosing schedule for Stelara. Your child’s doctor will determine their Stelara dose based on their body weight.
To learn more about Stelara’s dosage, see this article.
Your doctor will explain how you should take Stelara injections. They will also explain how much to inject and how often. Be sure to follow your doctor’s instructions. Below are commonly used doses, but always inject the dose your doctor prescribes.
Taking Stelara
Stelara comes as a solution inside prefilled syringes and single-dose vials. You’ll receive this solution as an injection under your skin.
Stelara solution for injection under your skin is available in two strengths:
- 90 milligrams/milliliter (mg/mL), in single-dose prefilled syringes
- 45 mg/0.5 mL, in single-dose prefilled syringes and single-dose vials
Stelara also comes as a solution inside single-dose vials that you’ll receive from healthcare professionals as an intravenous (IV) infusion. With an IV infusion, you’ll get the medication through your vein over a period of time.
Stelara solution for IV infusion is available in single-dose vials in one strength: 130 mg/26 mL.
Injection sites for Stelara
Your doctor or nurse will show you how to inject Stelara under your skin. Every time you inject Stelara, you should change the site of where you’re injecting the drug. You can choose from the following locations:
- outer side of your upper arms
- buttocks
- front of your thighs
- your abdomen, staying 2 inches (5 centimeters) away from your belly button
Taking Stelara with other drugs
You may need to take Stelara with other medications to treat your condition. Talk with your doctor if you have questions about taking other drugs together with Stelara.
Other drugs with Stelara for psoriasis or psoriatic arthritis
It’s not known if taking other immune system blockers or using phototherapy with Stelara for psoriasis is safe. But methotrexate may be used with Stelara to treat psoriatic arthritis if appropriate. It’s not known to interfere with the safety and efficacy of Stelara.
Other drugs with Stelara for Crohn’s disease or ulcerative colitis
For Crohn’s disease or ulcerative colitis, the following medications may be used with Stelara if appropriate:
- 6-mercaptopurine
- azathioprine
- methotrexate
These medications don’t affect the safety and effectiveness of Stelara. Also, if needed, your doctor may recommend that you use corticosteroids together with Stelara.
Questions about taking Stelara
Below, we answer some common questions about taking Stelara.
- What if I miss a dose of Stelara? If you forget to inject a dose of Stelara, take your dose as soon as you remember. If you’re unsure about when you should inject Stelara after missing a dose, talk with your doctor or pharmacist. They can help you set up a new schedule for your at-home injections.
- Will I need to use Stelara long term? The conditions that Stelara treats are long lasting diseases. So, you’ll likely need to take Stelara long term if it’s working well for you. Talk with your doctor to find out how long you’ll need to take Stelara. And don’t stop taking Stelara without first checking with your doctor. Stopping the drug may cause symptoms of your condition to come back. Once you stop taking Stelara, your doctor will monitor you to make sure you can safely stay off the treatment.
- Should I take Stelara with food? Stelara is taken as either an injection under your skin or an intravenous (IV) infusion. (With an IV infusion, you’ll get the medication through your vein over a period of time.) So, eating food doesn’t affect how your body absorbs it.
- How long does Stelara take to work? Everyone may have a different experience with Stelara treatment. And how long Stelara takes to work may depend on the condition it’s treating. For plaque psoriasis, you may have significant improvement in your symptoms after 12 weeks. For psoriatic arthritis, you may notice significant improvement after 24 weeks of treatment. But it’s possible that you’ll have improvement earlier. Stelara may work more quickly when it’s used for Crohn’s disease or ulcerative colitis.
Questions for your doctorYou may have questions about Stelara and your treatment plan. It’s important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
- Before your appointment, write down questions like:
- How will Stelara affect my body, mood, or lifestyle?
- Bring someone with you to your appointment if doing so will help you feel more comfortable.
- If you don’t understand something related to your condition or treatment, ask your doctor to explain it to you.
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, don’t be afraid to ask questions or offer feedback on your treatment.
Whether you have health insurance or not, cost may be a factor when you’re considering Stelara. What you’ll pay for Stelara may depend on several things, such as your treatment plan and the pharmacy you use.
If you have questions about how to pay for your prescription, talk with your doctor or pharmacist. A program called STELARA withMe may also be available.
You can also check out this article to learn more about saving money on prescriptions.
If you have certain autoimmune conditions, your doctor may prescribe Stelara for you. (With autoimmune diseases, your immune system is overactive.)
Stelara is used for the following long lasting diseases:
- Moderate to severe plaque psoriasis (PsO): For PsO, adults and children ages 6 years and older can take Stelara. With PsO, you have swollen, red or darkened patches on your skin. Over time, you may also develop swollen joints.
- Psoriatic arthritis (PsA): For PsA, adults and children ages 6 years and older can take Stelara. With PsA, you have red or darkened patches of skin and swollen joints. You may have arthritis in joints on both or just one side of your body. Usually, with this condition, you’ll develop skin issues before you develop joint swelling.
- Moderate to severe Crohn’s disease: For Crohn’s disease, adults can take Stelara. Crohn’s disease is a condition that affects the digestive system. With Crohn’s disease, you may have inflammation in any part of your digestive tract, from your mouth to your anus. You may have unpredictable times of remission, when your symptoms are managed. And you may have times of relapse, when your symptoms worsen.
- Moderate to severe ulcerative colitis (UC): For UC, adults can take Stelara. With UC, you have inflammation in your large intestine. With UC, you may have unpredictable times of remission, when your symptoms are managed. And you may have times of relapse, when your symptoms are worsened.
To manage symptoms of these long lasting diseases, your doctor may prescribe medications to slow down the activity of your immune system.
Stelara is an antibody (a type of protein) that’s made in a lab. It works by blocking substances made by your immune system that can cause long lasting inflammation. These substances, called cytokines, promote inflammation and may cause disease. By blocking cytokines, Stelara can help manage symptoms and relapses of certain diseases.
Find answers to some commonly asked questions about Stelara.
How does Stelara compare with Humira?
Both Stelara and Humira are biologic medications, which means they’re made from living cells.
Humira is only given as an injection under the skin. But Stelara can be given as an injection under the skin or as an intravenous (IV) infusion. (With an IV infusion, you’ll get the medication through your vein over a period of time.)
Adults can take either Stelara or Humira for:
Stelara can also be prescribed for children ages 6 years and older with plaque psoriasis and psoriatic arthritis. Humira is used for other diseases, too. These include rheumatoid arthritis in adults and juvenile idiopathic arthritis in some children.
Both Humira and Stelara target certain parts of your immune system. But each drug targets a different part:
- Humira blocks the action of a protein called tumor necrosis factor (TNF).
- Stelara blocks the action of proteins called interleukin-12 and interleukin-23.
The different ways these two drugs work may explain the differences in their side effects. For instance, unlike Stelara, Humira has a boxed warning for serious infections and cancer. (A boxed warning is the most serious warning given about a drug’s side effects.) Stelara may also cause serious infections and cancer. But it doesn’t have a boxed warning for these conditions.
If you’d like to know more about the differences between these two drugs, talk with your doctor or pharmacist or see this article.
Does Stelara cause weight gain?
No, Stelara doesn’t affect your weight.
On the other hand, if you’re taking Stelara for Crohn’s disease, the condition itself may cause weight loss.
If you’re losing or gaining weight while taking Stelara, talk with your doctor. They can help you determine what’s causing your weight to change. And they can suggest ways to help you manage a body weight that’s healthy for you.
If I stop taking Stelara, will I have withdrawal symptoms?
No, you won’t have withdrawal symptoms if you stop taking Stelara. Withdrawal symptoms are uncomfortable side effects that can occur when you stop taking a drug your body is used to.
But keep in mind that the symptoms of your condition may come back if you stop treatment. Once you stop taking Stelara, your doctor will monitor you to make sure you can safely stay off the treatment.
Be sure to talk with your doctor before stopping Stelara treatment.
Some important things to discuss with your doctor when considering Stelara include your general health and any medical conditions you may have. Other important things your doctor needs to know include whether you’re pregnant or considering pregnancy or breastfeeding.
Additionally, tell your doctor if you’re taking any prescription or over-the-counter (OTC) medications.
Interactions
Taking medications, vaccines, foods, and other things with a certain drug can affect how the drug works. These effects are called interactions.
Before taking Stelara, be sure to tell your doctor about all medications you take (including prescription and OTC types). Also describe any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Stelara.
For more information about Stelara and interactions, see this in-depth article.
Interactions with drugs or supplements
Stelara can interact with several types of drugs and therapies, including:
- the anticoagulant warfarin
- the immune system blockers cyclosporine and tacrolimus
- allergy shots for people with severe allergies
This list doesn’t contain all types of drugs that may interact with Stelara. Your doctor or pharmacist can tell you more about these interactions and any others that may occur with use of Stelara.
Other interactions
Before starting Stelara, you should make sure your vaccinations are up to date. Ask your doctor which vaccines you need to receive. Once you start taking Stelara, your body may not respond as well to vaccines.
During treatment with Stelara, you can’t receive any live vaccines. Live vaccines contain weakened forms of live germs. While you’re using Stelara, your immune system’s activity is lowered. So, live vaccines may cause you to get the infection they were meant to protect you from. Receiving a live vaccine during Stelara treatment increases your risk of serious infections.
Examples of live vaccines include:
Also, you shouldn’t receive the bacillus Calmette-Guérin (BCG) vaccine from one year before starting Stelara until one year after stopping the drug. (The BCG vaccine is meant to protect you from tuberculosis.) If you need a BCG vaccine, ask your doctor about when you can get it.
When you’re using Stelara, it’s also important that your household members be careful about getting live vaccines. The person who receives the live vaccine may shed some of the live germ from it. And this could cause you to become ill.
Warnings
Stelara may not be right for you if you have certain medical conditions or other factors that affect your health. Talk with your doctor about your health history before you take Stelara. Factors to consider include those in the list below.
- Serious infections: Your doctor will not prescribe Stelara for you if you have an active infection. This is because getting the drug might make the infection worse. Your doctor may need to treat your infection before having you start Stelara. Some people have developed serious, and sometimes rare, infections while taking Stelara. If your body doesn’t make enough of an immune system protein called interleukin-12 or interleukin-23, you have a higher risk of infection. Your doctor will evaluate your risks before prescribing Stelara for you. If you notice any symptoms of infection while you’re taking Stelara, tell your doctor right away.
- Allergic reaction: If you’ve had an allergic reaction to Stelara or any of its ingredients, you shouldn’t take Stelara. Ask your doctor what other medications are better options for you.
- Tuberculosis (TB): Before starting Stelara, your doctor will test you for TB. It’s possible to have latent TB, which means that you’re not ill but you have TB in your body. Taking Stelara can make latent TB become active and cause symptoms. If you have TB, your doctor may treat it before prescribing Stelara for you.
- Cancers: Stelara lowers the activity of your immune system. This may increase your risk for certain cancers, including skin cancer. Before starting Stelara, tell your doctor if you’ve ever had cancer.
Use with alcohol
Some medications interact with alcohol, but Stelara doesn’t. If you drink alcohol, ask your doctor if it’s safe to drink it during your treatment with Stelara.
Pregnancy and breastfeeding
If you can become pregnant or are breastfeeding, it’s important to consider whether Stelara is a safe choice for you.
You can also refer to this article for more information. If you have other questions, talk with your doctor.
Don’t take more Stelara than your doctor prescribes. Using more than this can lead to serious side effects.
If you inject more Stelara than what’s prescribed, your doctor will closely monitor you for any symptoms of overdose.
What to do in case you take too much Stelara
Call your doctor if you think you’ve taken too much Stelara. You can also call 800-222-1222 to reach America’s Poison Centers or use its online resource. However, if you have severe symptoms, immediately call 911 (or your local emergency number) or go to the nearest emergency room.
Q:
Which creams can I use for plaque psoriasis while using Stelara?
AnonymousA:
Your doctor may have you use Stelara together with a topical cream to treat plaque psoriasis. Topical products can help reduce the scaling, itching, and discomfort of this condition. Both over-the-counter and prescription topical products are available in various forms, including creams, lotions, and ointments.
When choosing a topical product, it’s best to avoid ones with fragrances and dyes. They can irritate your skin. Also, watch for herbal or natural ingredients, such as tea tree oil or aloe vera. There isn’t enough information available to know how safe they are and how well they work in treating plaque psoriasis.
A variety of creams for psoriasis are available. Look for these ingredients, which can help treat psoriasis:
- retinoids
- coal tar
- synthetic vitamin D
- anthralin
- salicylic acid
- corticosteroids
- calcineurin inhibitors
Psoriasis affects everyone differently, so some topical products may work better for you than others. Talk with your doctor or pharmacist to find a topical treatment that is suitable for you. And always be sure to check with your doctor before starting any new topical product.
The Healthline Pharmacist TeamAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.